Learn how you can identify gastroparesis symptoms with the help of BetterHealthCare.com.
Have you ever asked, what is diabetic gastroparesis? If you are diabetic, you should be aware that diabetes can cause gastroparesis. This medical condition affects the efficacy of the stomach to move food into the small intestine. When food is blocked from leaving the stomach area, you can experience heartburn, nausea and bloating. These are just some of the gastroparesis symptoms that can make a good day go sour.
Click here to see the relationship between CBD oil and diabetes.
What is Diabetic Gastroparesis?
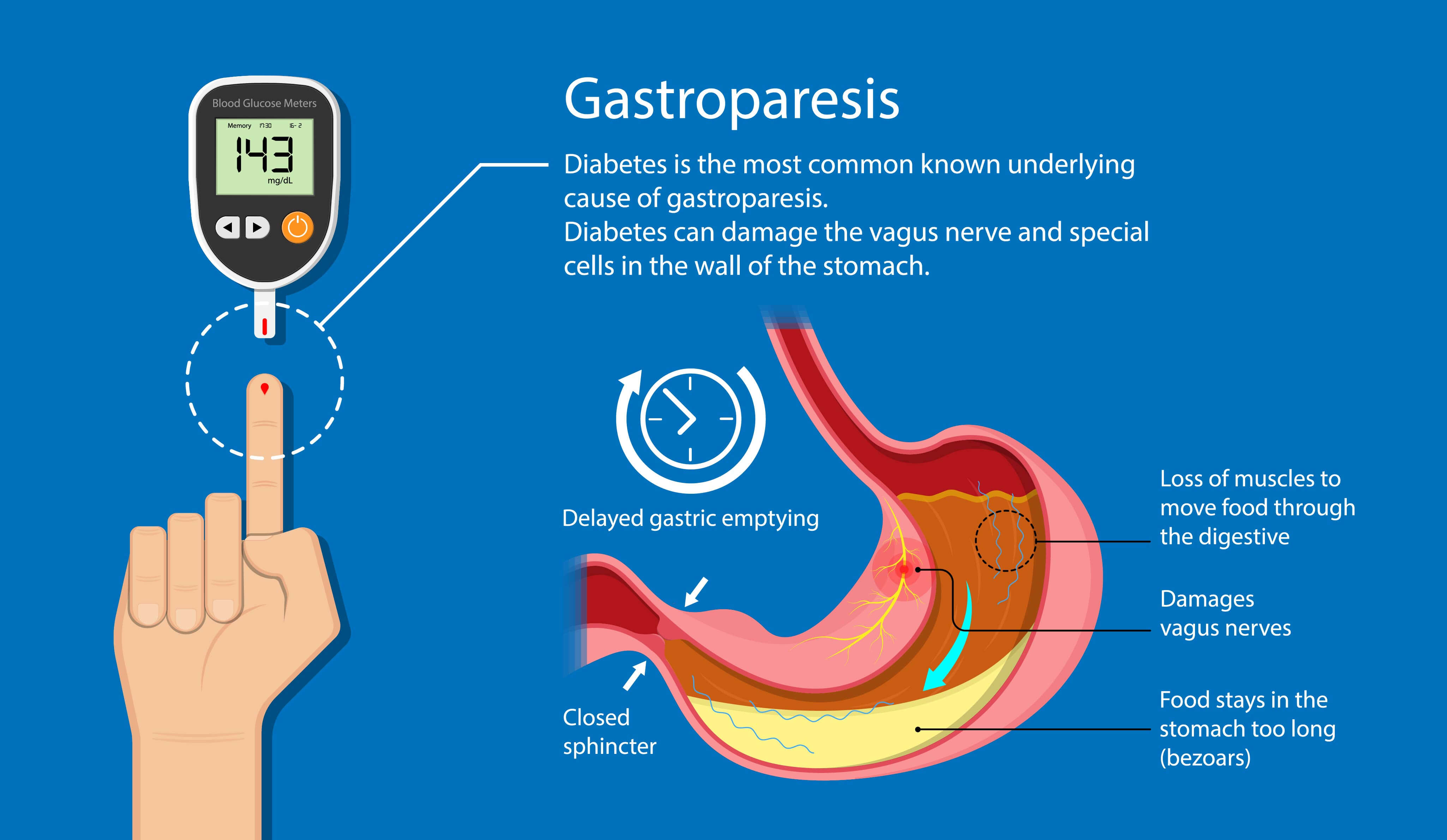
What is diabetic gastroparesis and how does it affect the stomach? Diabetic gastroparesis literally means “stomach paralysis” and is a digestion problem that prevents the stomach from contracting. The stomach muscles must contract to break down food and send it to the small intestines, where food is further digested and nutrients are absorbed. In healthy digestion, the vagus nerve sends neurotransmitter impulses to the smooth stomach muscle so that it begins to contract and digest food. Diabetic gastroparesis prevents this from occurring.
Diabetes type 1 and 2 can have a direct effect on the nervous system, and cause nerve damage. The vagus nerve can be damaged by diabetes, and cause the stomach muscles to stop operating normally. This health problem, also known as “delayed emptying” slows down or prevents food from being digested and being moved to the small intestine.
Do you Have Gastroparesis Symptoms?
If you have diabetic gastroparesis, you may begin to experience some of the following gastroparesis symptoms:
- Heartburn, bloating, indigestion, epigastric pain
- Loss of appetite, feeling full after eating a small amount of food
- Unexplained weight loss
- Unstable blood sugar levels
- Stomach spasms
- Gastroesophageal reflux
- Nausea, vomiting, especially if food is undigested.
Gastroparesis symptoms can occur anytime after eating, especially after ingesting:
- Solid foods
- Fatty foods
- High fiber foods like raw fruits and vegetables
- Carbonated drinks
Regurgitation and vomiting can occur many hours after eating. Weight loss can occur because of a lack of calories being absorbed, and poor health can occur because nutrient absorption has been prevented.
What is a Diabetic Gastroparesis Risk Factor?
Diabetics are at a greater risk of developing gastroparesis than people who do not have diabetes. Other risk factors include:
- Having Type 1 diabetes
- Having Type 2 diabetes for more than 10 years
- Having a history of gastric surgeries that could have affected the vagus nerve
- Having a co-existing autoimmune disease
- Radiation treatment
- Eating disorders
- Certain types of cancer
- Infections
- Neuromuscular diseases
- Narcotics and medications
What are Diabetic Gastroparesis Complications?
Diabetic gastroparesis makes it harder to manage blood sugar levels in diabetics. The unpredictability of when food will move out of the stomach and into the small intestine makes it harder for diabetics to figure out when to take their insulin. When blood sugar is too high or too low, serious health complications can arise, such as:
- Eye damage, cataracts, retinopathy
- Ketoacidosis, malnutrition
- Bacterial infections
- Electrolyte imbalance
- Neuropathy
- Heart disease
- Kidney damage
- Serious foot problems leading to amputation
- Difficulty swallowing
- Diabetic coma
- Shaking, loss of consciousness
- Seizures
Gastroparesis Treatment
The most important gastroparesis treatment is keeping your blood sugar in a safe range. This will require the diabetic to test their blood sugar more often. Other gastroparesis treatments can include:
- A change in diet and eating habits
- Avoiding drugs, such as opiates, that delay stomach emptying
- Changing the time and dosage of taking insulin
- Taking medications that stimulate the stomach muscles, assist digestion, and combat nausea
- Eating well-balanced, more nutritious smaller meals, more frequently
- Limiting high fiber foods
- Eating low-fat foods, and cooked vegetables
- Eliminating alcohol and carbonated beverages
Click here to discover the first signs of type 2 diabetes.
A change in eating habits is a must for anyone with diabetic gastroparesis. Ask your doctor or nutritionist to help you prepare a meal plan and recommend medications for suitable gastroparesis treatment.
Learn more at BetterHealthKare.com